Abstract Code: IUC24415-81
Clinical outcomes in stage I seminoma patients aged ≥ 45 years according to treatment modality
F. Mascaro 1, A. Marmiroli 2, A. Nuzzo 2, M. Maruzzo 3, D. Bimbatti 3, S. Nazzani 2, M. Claps 2, G. Procopio 2, N. Nicolai 2, P. Giannatempo 2
(1) Università degli Studi di Pavia, Pavia – Italy, (2) Fondazione IRCCS Istituto Nazionale dei Tumori, Milano – Italy, (3) Istituto Oncologico Veneto, Padova – Italy
Background: Data regarding progression-free (PFS) and overall survival (OS) in clinical Stage I (CSI) seminomatous germ-cell tumors (SGCT) patients older than 45 years are limited. We address this knowledge gap, testing for these clinical outcomes according to treatment modalities within retrospective multicenter real-world data from three Italian institutions.
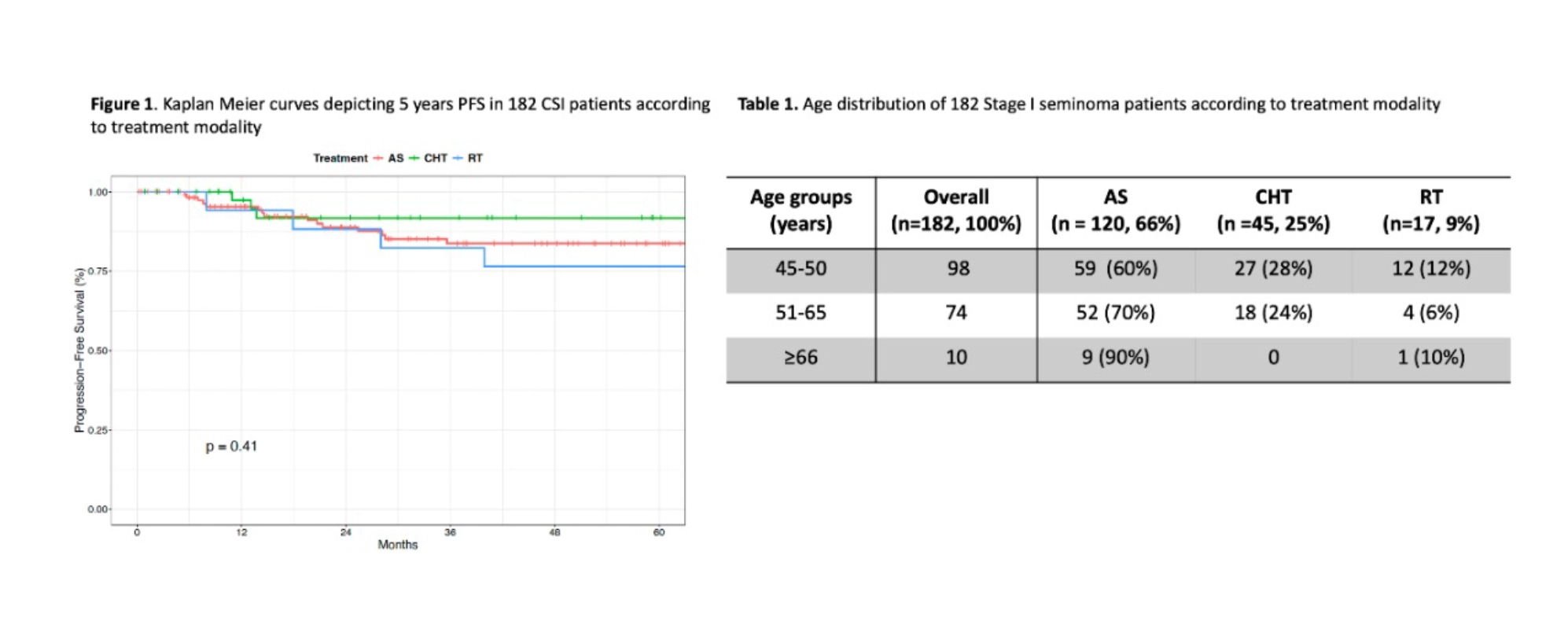
Methods: Data from patients aged ≥ 45 years diagnosed with testicular CSI SGCT between 01/1992 and 07/2023 were collected. Descriptive analyses were performed and Kaplan-Meier curves were used to assess PFS and OS according to treatment modality, consisting of active surveillance [AS] vs. adjuvant chemotherapy [CHT: 1 course of carboplatin AUC 7] vs. adjuvant radiotherapy [RT: 20 to 30 Gy as paraortic strip or paraortic plus ipsilateral iliac nodes]).
Results: A total of 182 patients were selected. Of those, 120 (65%) underwent AS, 45 (25%) CHT, and 17 (10%) RT. Overall median age was 49.6 years (IQR 46.4–54.6). Patients undergoing AS were older (50.2 yo, IQR 47.2–55.3) than patients undergoing CHT (49.3 yo, IQR 46.4–51.3) or RT (49.3 yo, IQR 45.1–49.7). Most patients (98/182 or 54%) were aged between 45 and 50 years: 59 (60%), 27 (28%) and 12 (12%) underwent AS, CHT and RT, respectively. Patients aged 51–65 were 74 (41%): 52 (70%), 18 (25%) and 4 (5%) underwent AS, CHT and RT, respectively. Ten patients (5%) were aged >65: 9 underwent AS and 1 RT. (Table 1). After a median follow-up of 60 months, 5-year PFS was 83.7% for AS, 91.7% for CHT and 76.5% for RT (p=0.41) (Figure 1). Relapses occurred in 18 (15%) vs. 4 (9%) vs. 5 (29%) patients in AS vs. CHT vs. RT, respectively. After a median follow-up of 60 months, 5-year OS was 100% across all treatment groups (p= 0.47).
Conclusions: In CSI SGCT patients aged over 45, outcomes were excellent and aligned with the general CS I SGCT population, with 5-year PFS differences among treatment groups not reaching statistical significance. All relapsed patients were cured, and the 5yrs OS reached 100%. These results confirm the favorable prognosis of CSI SGCT even in older men.